Obesity is linked to numerous serious health conditions and complications, affecting nearly every organ system in the body. These include:
Cardiovascular
Arterial Hypertension
Obesity is a leading risk factor for high blood pressure, with approximately 75% of hypertension cases directly linked to excess weight. Hypertension significantly increases the likelihood of developing severe conditions such as coronary heart disease, congestive heart failure, stroke, and kidney disease.
Varicose Veins and Phlebitis
Varicose veins are characterized by dilated veins that impede efficient blood flow back to the heart, a condition caused by malfunctioning venous valves. This leads to blood pooling in the veins, causing them to enlarge.
Phlebitis refers to inflammation in a vein. When this inflammation is caused by a blood clot partially or entirely blocking the vein, it is called thrombophlebitis. This condition can occur superficially in veins close to the skin or in deeper veins below the dermal layers.
Venostasis in the Lower Extremities
Venostasis, or venous stasis, occurs when blood flow in the veins slows down, typically in the legs. This condition increases the risk of thrombi (blood clots) forming in the veins, which can lead to deep vein thrombosis (DVT). DVT is particularly dangerous because clots in deep veins can travel to the lungs, causing a potentially life-threatening pulmonary embolism.
Cardiac Decompensation
Heart disease remains a leading cause of death, claiming approximately 600,000 lives annually in the United States alone. Obesity is recognized by the American Heart Association as a significant risk factor for heart disease. Research shows that the risk of coronary heart disease increases in correlation with obesity, particularly severe obesity. This condition not only raises the likelihood of heart attacks but also contributes to heart failure and irregular heart rhythms (arrhythmias). Severe arrhythmias can triple the risk of cardiac arrest. Interestingly, some studies suggest that mild excess weight may offer protective benefits against mortality following a heart failure diagnosis.
Arteriosclerosis
Arteriosclerosis, often referred to as atherosclerosis, occurs when the arteries that transport oxygen and nutrients from the heart to the body become thickened and stiff, reducing blood flow to organs and tissues. While healthy arteries are flexible and elastic, obesity accelerates the hardening of arterial walls, a condition that can severely impair cardiovascular health.
Managing obesity effectively is crucial for reducing these risks and preventing the progression of these potentially life-threatening conditions.
Respiratory
The Impact of Obesity on Respiratory Health
Excess body fat can place significant strain on the respiratory system. Increased fat levels elevate the body’s demand for oxygen while simultaneously reducing lung capacity, making breathing more difficult. This explains why many individuals with obesity experience a sense of suffocation or breathlessness during physical exertion.
People with obesity are at higher risk of respiratory conditions, including infections, asthma, and other breathing disorders. In fact, studies indicate that asthma is three to four times more prevalent in individuals with obesity.
Key Respiratory Conditions Linked to Obesity
1. Pickwickian Syndrome (Obesity Hypoventilation Syndrome, OHS):
This serious respiratory condition occurs in people with obesity and is characterized by low oxygen levels and elevated carbon dioxide levels in the blood. OHS is caused by chronic hypoventilation, particularly during the day. Its three primary features include:
- Obesity
- Daytime hypoventilation (reduced ability to expel carbon dioxide)
- Sleep-disordered breathing, such as obstructive sleep apnea (OSA)
Also known as Pickwickian syndrome, it takes its name from Charles Dickens’ depiction of similar symptoms in The Pickwick Papers.
2. Obstructive Sleep Apnea (OSA):
OSA is a serious respiratory condition affecting 50–60% of people with obesity and up to 90% of those with severe obesity. It occurs when excess fat in the neck, throat, or tongue obstructs the airways during sleep. This leads to apnea episodes, where breathing temporarily stops.
- These episodes can occur hundreds of times a night, reducing blood oxygen levels and disrupting restful sleep.
- Untreated OSA can result in severe complications, including high blood pressure, pulmonary hypertension, heart failure, stroke, and even sudden cardiac death.
- Fatigue and daytime drowsiness caused by OSA can also increase the risk of car accidents.
3. Chronic Drowsiness and Hypersomnia:
The low oxygen levels caused by obesity-related breathing disorders can lead to extreme tiredness and excessive daytime sleepiness (hypersomnia). This fatigue can significantly impair daily functioning and overall quality of life.
4. Bronchitis:
Obesity increases the likelihood of inflammation in the lower airways, such as the bronchial tubes, resulting in bronchitis. This condition can occur due to infection or other irritants, causing coughing, wheezing, and discomfort.
5. Pulmonary Secretions and Embolism:
Obesity can lead to an accumulation of pulmonary secretions, impairing lung function. Additionally, the risk of pulmonary embolism—a potentially life-threatening condition where a blood clot blocks the lungs’ blood vessels—is elevated in people with obesity.
Takeaway
The respiratory challenges associated with obesity extend beyond breathlessness. Conditions like OSA, Pickwickian syndrome, and bronchitis can have life-altering consequences if left untreated. Addressing obesity through medical intervention, lifestyle changes, or weight management strategies is critical to improving respiratory health and reducing the risk of serious complications.
Digestive
Gallbladder Stones
Gallbladder stones, or gallstones, are hardened deposits that form in the gallbladder, often causing pain, nausea, and digestive problems. These stones can vary in size and may obstruct bile flow, leading to inflammation or infection. Severe cases may require surgical intervention to remove the gallbladder.
Liver Cirrhosis
Liver cirrhosis is the progressive scarring of the liver tissue caused by long-term liver damage. As the liver becomes scarred, its ability to function deteriorates, disrupting vital processes such as detoxification and metabolism. Cirrhosis is a leading cause of illness and death in the United States, affecting about 5.5 million people, or 2% of the population. With 26,000 deaths annually, it ranks as the seventh leading cause of death among adults aged 25 to 64. The number of individuals affected by cirrhosis is expected to rise as risk factors like alcohol abuse and chronic hepatitis continue to impact public health.
Gastroesophageal Reflux and Heartburn
Gastroesophageal reflux disease (GERD) occurs when stomach acid or intestinal contents flow backward into the esophagus, irritating the lining and causing discomfort. Symptoms commonly include heartburn, indigestion, regurgitation, coughing (especially at night), hoarseness, and excessive belching. GERD affects 10–20% of the general population regularly, and its prevalence has been linked to risk factors such as obesity, which increases the likelihood of developing GERD, erosive esophagitis, and, in rare cases, esophageal cancer (adenocarcinoma).
Pancreatitis
Pancreatitis is the inflammation of the pancreas, often triggered by gallstones, alcohol abuse, or other factors that disrupt normal pancreatic function. This condition can range from mild to severe and may lead to complications such as organ failure or infection. Acute pancreatitis requires urgent medical attention, while chronic pancreatitis can lead to lasting damage and digestive problems.
Mechanical and Motor
Obesity, especially in its severe form, significantly contributes to a variety of bone and joint issues, which can increase the risk of accidents and personal injury. These conditions place additional stress on the body, leading to chronic pain and mobility challenges. Common bone and joint problems associated with obesity include:
- Joint Diseases: Conditions such as osteoarthritis and gout, which result from excessive wear and tear on the joints, are more prevalent in individuals with obesity.
- Herniated Disc: Excess weight can place added pressure on the spine, increasing the likelihood of a herniated disc, which may cause intense pain and nerve damage.
- Spinal Disorders: Obesity can contribute to various spinal issues, including misalignments and conditions like scoliosis or kyphosis, that impair posture and cause discomfort.
- Back Pain: The added weight strain on the spine and surrounding muscles often leads to chronic back pain, which can impact everyday activities and mobility.
- Osteoarthritis of the Hip and Knees: The weight-bearing joints, especially the hips and knees, are at greater risk of developing osteoarthritis, causing pain, stiffness, and difficulty moving.
- Osteoarthritis and Deformation of the Spine: The cumulative effects of obesity on spinal health can lead to osteoarthritis and deformities, further limiting flexibility and increasing discomfort.
Addressing obesity is crucial not only for improving overall health but also for reducing the risk of these debilitating bone and joint conditions.
Endocrine
Type 2 Diabetes: A Chronic and Progressive Disease
Type 2 diabetes (T2DM) is a complex, chronic, and progressive disease with multifactorial origins. It involves disturbances in the metabolism of carbohydrates, fats, and proteins, and is primarily characterized by a combination of insulin resistance and either a relative or absolute deficiency in insulin. The hallmark of the condition is hyperglycemia, or elevated blood glucose levels.
Obesity, especially when marked by visceral fat accumulation, plays a significant role in the development of T2DM. Individuals genetically predisposed to inflammatory and metabolic mechanisms are at a higher risk of developing the disease, often leading to a cascade of health complications, including cardiovascular disease.
The Link Between Obesity and Type 2 Diabetes
Obesity is one of the leading causes of T2DM. People with severe obesity are approximately 10 times more likely to develop type 2 diabetes compared to those of a healthy weight. Additionally, T2DM can nearly double the risk of premature death. If left unmanaged, the disease can lead to a range of serious health complications, including:
- Amputations
- Heart disease
- Stroke
- Blindness
- Kidney disease
- High blood pressure
- Nerve damage and circulatory issues
- Chronic infections that are difficult to treat
- Impotence
Prediabetes: A Critical Stage
Prediabetes is a condition where individuals have blood glucose levels higher than normal but not yet high enough to be classified as T2DM. This stage increases the risk of developing full-blown diabetes and its associated complications, both macrovascular (e.g., heart disease) and microvascular (e.g., kidney damage, nerve problems).
Metabolic Syndrome: A Convergence of Risk Factors
Metabolic syndrome (MS) is a collection of metabolic abnormalities that increase the risk of cardiovascular diseases and diabetes. The primary underlying factors are abdominal obesity and insulin resistance, which together serve as the pathophysiological foundation of the syndrome. MS is now recognized as a distinct pathological condition characterized by the convergence of several risk factors, such as:
- Insulin resistance
- Glucose intolerance or type 2 diabetes
- Dyslipidemia (abnormal lipid levels)
- Thrombosis (increased blood clotting risk)
- Chronic inflammation
- Hypertension (high blood pressure)
- Central obesity
In addition to these, metabolic syndrome can also contribute to:
- Menstrual disorders in women
- Erectile dysfunction in men
- Infertility
The increasing prevalence of metabolic syndrome underscores the urgent need for preventive measures and effective management to reduce the burden of both T2DM and cardiovascular disease globally.
Dermatological
Dermatological Concerns
Fungal Infections: Skin infections caused by fungi that often present as red, itchy patches, typically in moist areas of the body. These infections can cause discomfort and require appropriate antifungal treatment.
Red Spots and Irritation in the Joints: The appearance of red spots or irritated patches around the joints can be a sign of an underlying skin condition or infection. These areas may become inflamed, itchy, or painful and may require medical evaluation to determine the cause.
Cuts or Breaks in the Skin: Small or large breaks in the skin that can result from injury, irritation, or infection. If left untreated, these can lead to further complications, such as infections, scarring, or prolonged healing.
Leg Swelling and Skin Ulcers: Swelling in the legs, often accompanied by the formation of open sores (ulcers) on the skin, can indicate poor circulation, chronic venous insufficiency, or other circulatory issues. These ulcers may be painful and prone to infection, requiring prompt medical attention to promote healing and prevent complications.
Psycho-social
Psycho-Social Impact of Obesity
Obesity can significantly affect an individual’s psychological and social well-being, leading to a range of challenges in daily life and personal interactions. These include:
- Difficulty Dressing: Struggling to find clothes that fit comfortably or align with personal style can affect self-esteem and body image.
- Inability to Follow Fashion Trends: Limited clothing options can make it challenging to keep up with current fashion trends, contributing to feelings of frustration or exclusion.
- Impact on Relationships: Obesity in one partner can strain emotional and sexual relationships, potentially leading to feelings of distance or dissatisfaction.
- Social Stigma: Individuals with obesity may face negative comments or impertinence from others, both from close relationships and strangers, which can result in emotional distress.
- Nervous Breakdown: The emotional toll of living with obesity, including social rejection or self-consciousness, can lead to anxiety, stress, and even breakdowns.
- Negative Self-Perception: Many individuals with obesity feel different or “othered,” often in a negative way, which can affect their sense of self-worth.
- Social Withdrawal: Feelings of shame or self-consciousness may lead some to isolate themselves, avoiding social situations and further exacerbating loneliness.
- Job Insecurity: Obesity can also affect one’s ability to work effectively, leading to potential maladjustment in the workplace or challenges in maintaining a career.
- Employment Challenges: Individuals with obesity may face difficulties securing or retaining employment due to biases or perceived limitations, impacting their economic stability and career growth.
These psycho-social factors highlight the importance of addressing obesity not only for physical health but also for emotional and social well-being, as it can have a profound effect on self-image, relationships, and overall quality of life.
Other Consequences
Other Serious Consequences of Obesity
Stress Urinary Incontinence
Obesity can increase the pressure on the pelvic organs, leading to stress urinary incontinence. This condition involves the involuntary leakage of urine during activities that put pressure on the bladder, such as coughing, sneezing, or exercise.
Idiopathic Intracranial Hypertension (IIH)
This condition, also known as pseudotumor cerebri, involves increased pressure in the brain without an obvious cause, such as a tumor. Obesity is a major risk factor for IIH, which can lead to headaches, vision problems, and, if untreated, permanent vision loss.
Alzheimer’s Disease and Cognitive Decline
Research has shown that obesity during middle age can significantly contribute to the development of Alzheimer’s disease and other forms of dementia later in life. The link between obesity and cognitive decline is thought to involve inflammation and other metabolic changes that impact brain health.
Renal Disease
Obesity contributes to several conditions that increase the risk of kidney disease and kidney failure, including hypertension, type 2 diabetes, and congestive heart failure. These conditions are often worsened by obesity and can lead to the gradual deterioration of kidney function.
Mental Health and Suicide Risk
Severe obesity is associated with an increased risk of major depressive disorder due to factors like physical and social discrimination. While studies on the link between obesity and suicide are mixed, most suggest that people with obesity tend to have lower suicide rates. However, obesity-related depression remains a serious concern.
Septicemia
Septicemia, a life-threatening infection, can lead to septic shock and death if not promptly treated. People with severe obesity are at a heightened risk of developing septicemia, likely due to compromised immune function and the increased likelihood of infection in the presence of other obesity-related conditions.
Liver Disease
Obesity is the primary cause of nonalcoholic fatty liver disease (NAFLD), a condition where fat builds up in the liver without alcohol consumption. NAFLD can progress to liver scarring, known as cirrhosis, which impairs liver function and can lead to liver failure if left untreated.
Obesity and Cancer Risk
Obesity is a significant risk factor for many types of cancer, including breast, colon, and pancreatic cancer. It is believed that obesity contributes to up to 90,000 cancer-related deaths annually in the United States alone. As your body mass index (BMI) rises, so does your risk of developing cancer and dying from it. For individuals with severe obesity, the cancer-related death rate increases by 52% for men and 62% for women.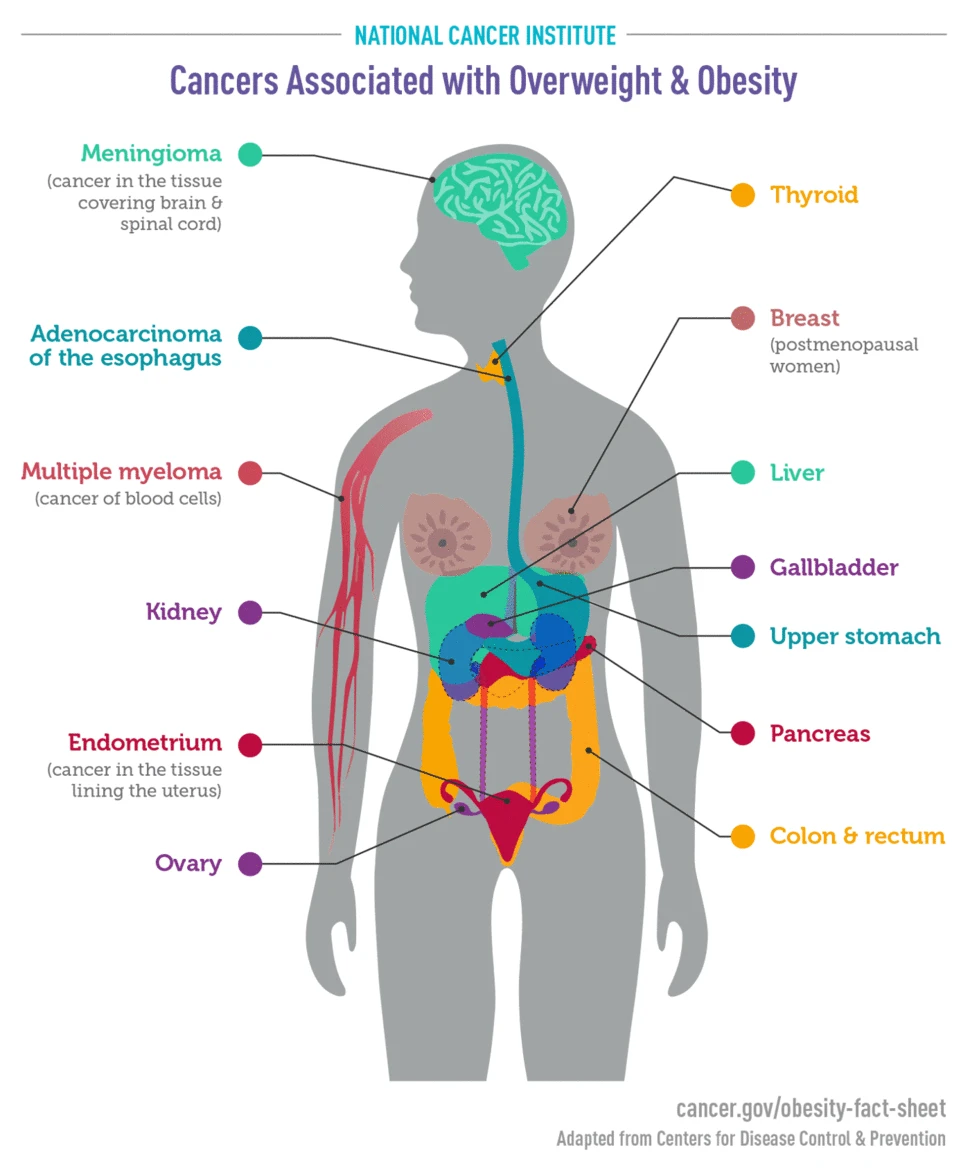
Ref: National Cancer Institute
Cerebrovascular Disease and Stroke
Obesity places significant stress on the circulatory system, increasing the risk of cerebrovascular diseases such as stroke. Obesity is often linked to several risk factors for stroke, including heart disease, hypertension, metabolic syndrome, type 2 diabetes, lipid abnormalities, and obstructive sleep apnea. These factors, combined with the added pressure from obesity, significantly elevate the likelihood of stroke.
Conclusion
Obesity has profound and wide-reaching effects on your health, contributing to a host of conditions that can severely impact your quality of life and longevity. However, the good news is that many obesity-related complications can be mitigated or even reversed through weight loss and lifestyle changes. Addressing obesity proactively can significantly reduce the risk of these life-threatening diseases.



